Introduction
Fat embolism (FE) refers to the presence of fat globules in the pulmonary or peripheral circulation. FE occurs frequently after trauma, particularly with fractures of the long bones in the lower extremities or orthopedic procedures involving bone marrow manipulation. FE syndrome (FES) is defined as the clinical symptoms and signs of organ dysfunction caused by the obstruction of capillaries by fat emboli and subsequent inflammatory reaction. The classical triad of respiratory distress, neurologic symptoms, and petechial hemorrhages occurs 24–72 h after an asymptomatic period. The diagnosis relies on clinical suspicion, symptoms, laboratory results, and imaging findings. The treatment is mainly supportive, and prevention with early stabilization of the fracture site is important [1]. Herein, we report a case of FES occurring after a femur shaft fracture in a level I trauma center.
Case presentation
A 27-year-old man without a past medical history was admitted to the trauma center after an in-car traffic accident. Although he was alert, his vital signs included a blood pressure of 75/59 mmHg, pulse rate of 103 beats per minute, respiratory rate of 30 breaths per minute, and body temperature of 36.2oC. He was diagnosed with grade 3 spleen laceration, grade 2 liver laceration, and intraperitoneal bladder rupture. A pelvic ring fracture with disruption of the posterior arch and left femur shaft fracture were also noted. He underwent emergency surgery for the primary repair of the bladder and splenic and hepatic hemostasis by a trauma surgery team. The postoperative hemodynamics was stable.
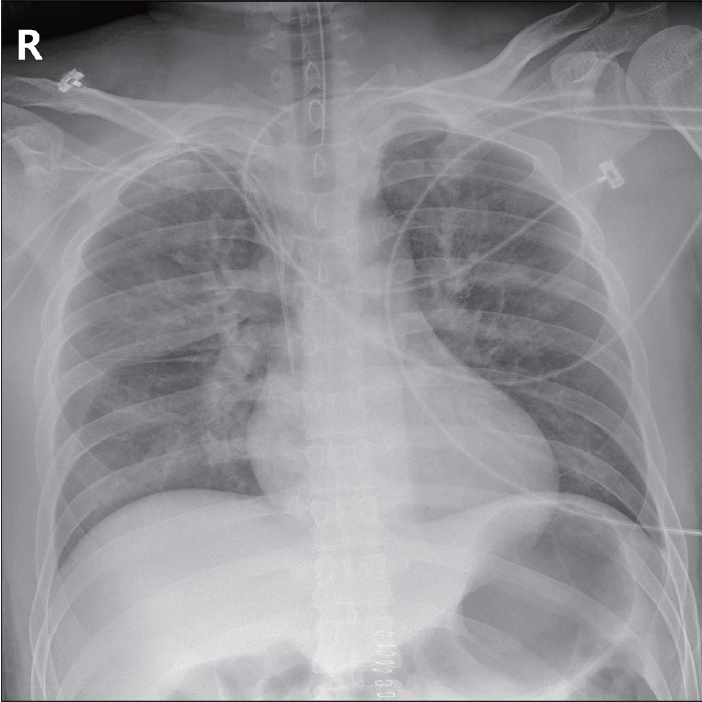
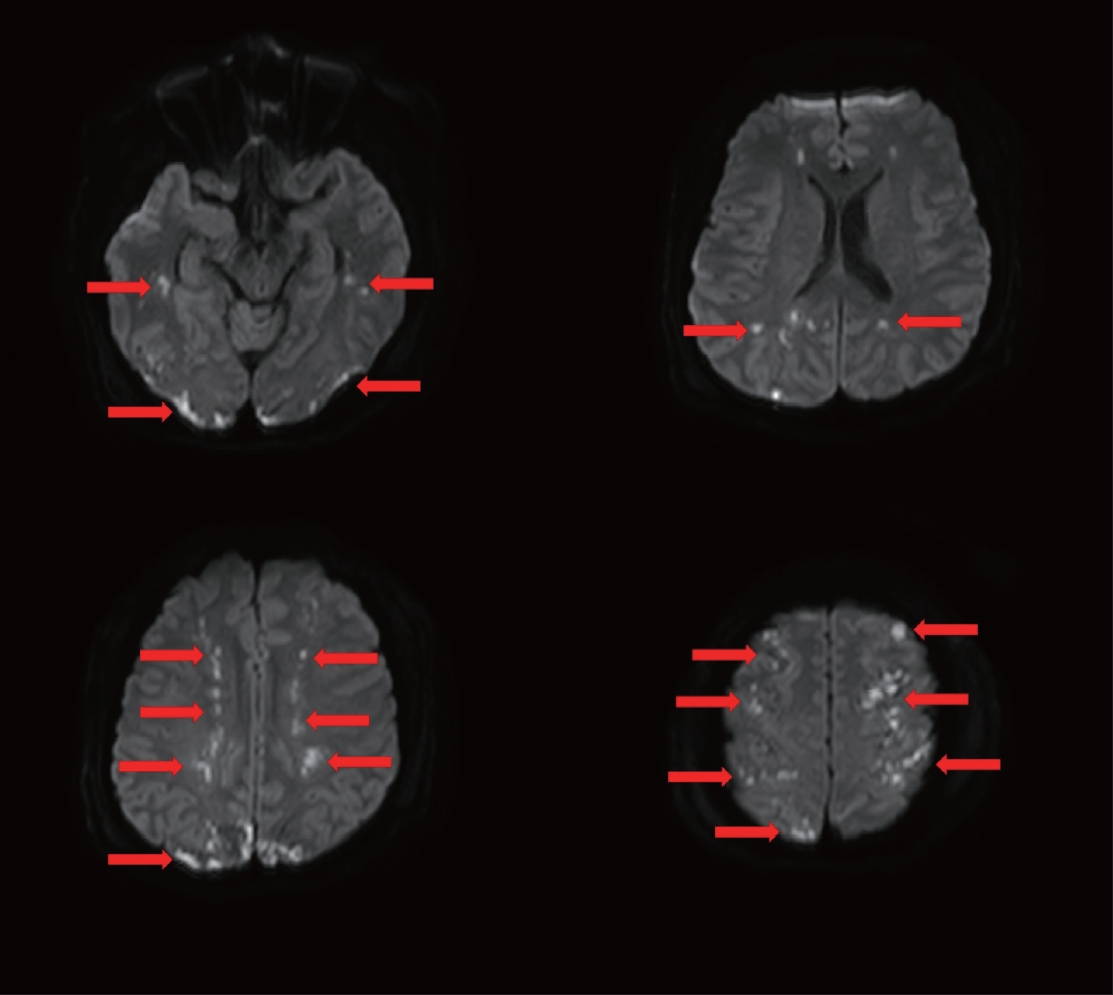
On postoperative day (POD) 2, blood gas analysis revealed dyspnea, tachypnea, and hypoxemia. The patient underwent endotracheal intubation, and bilateral pulmonary edema was noted on the chest radiograph (Fig. 1). Since the mental status deteriorated to a Glasgow coma scale (GCS) of E2M4Ve on the same day, computed tomography (CT) of the brain was performed. Although no remarkable abnormalities were noted until POD 3, multifocal ischemic changes were suspected in brain CT on POD 4. Water-diffusion magnetic resonance imaging (MRI) revealed diffusely scattered hyperintense signal abnormality in the bilateral cerebral hemisphere (Fig. 2). In addition, the patient presented left subconjunctival petechiae.
As FES was confirmed by the author’s team, the patient underwent orthopedic surgery for the stabilization of the pelvic and femoral fractures on the next day. The treatment of FES was primarily supportive of pulmonary edema and cerebral infarction. The patient was extubated, and the GCS improved to E4M6V5 on POD 10.
Discussion
Several hypotheses have been proposed about the etiology and pathophysiology of FES, which have not been identified. According to a study using the National Hospital Discharge Survey of the United States, FES occurs in 0.54% of isolated femoral fractures and 1.29% of multiple femoral fractures [2]. Several criteria, e.g., Gurd’s or Schonfeld’s [3,4], are sometimes used to diagnose FES. Of these, cerebral involvement, respiratory insufficiency, and petechial rash are the major criteria. Moreover, brain MRI is a sensitive imaging technique for diagnosing cerebral involvement and severity of damage in FES. On diffusion-weighted MRI, FES shows multiple hyperintense signal abnormalities in the bilateral cerebral hemispheres, also known as a “starfield pattern” [5]. This patient was diagnosed with FES because he had fractures of the pelvic ring and femoral shaft and showed the characteristic triad of pulmonary edema, neurologic distress with cerebral infarction, and subconjunctival petechiae.
Given the lack of standard treatment for FES, symptomatic and supportive care is provided. Several studies have used heparin, increased fluid, aspirin, and corticosteroids as treatment options; however, their effects are unclear. As direct treatment options for FES are scarce, prevention is paramount. A randomized control trial reported that the occurrence of FES could be reduced by the prophylactic administration of corticosteroids; however, routine prophylaxis is not recommended owing to the lack of high-quality evidence [1]. A study reported that earlier surgical fixation results in a lower incidence of FES in pelvic or long bone fractures [6]. In the present case, the orthopedic surgery team performed the fixation of pelvic and femoral fracture sites in order to prevent the aggravation of FES, despite the evidences that incipient fixation of fracture inhibits deterioration of already diagnosed FES are scarce. Therefore, more studies are needed on the treatment and prevention of FES.