Traumatic Atlanto-Occipital Dislocation: Two Cases
Article information
Abstract
Traumatic atlanto-occipital dislocation (AOD) is caused by high-energy trauma, such as a traffic accident or a fall from a height, and is essentially a rare cervical spine injury that is mostly fatal. A majority of patients with AOD either immediately die or survive for a few hours or days only, mostly owing to the accompanying injuries to the brain stem and lesions of the vascular structures of the neck. Here, we report two patients with AOD, who arrived alive at the hospital, but immediately proceeded to a cardiac arrest and death.
CASE
Two females aged 67 and 29 years were admitted with comatose mentality and sustained blunt trauma from a traffic accident and a fall, respectively. Both patients had a cardiac arrest at the accident scene, and return of spontaneous circulation was achieved after cardiopulmonary resuscitation. The injury severity scores were 38 and 75, respectively, without massive bleeding focus. Upon arrival at the hospital, the initial hemodynamics of both the patients were unstable with a pulse rate of 128 and 80 beats/min and a blood pressure of 79/64 and 39/22 mm Hg, respectively. The first patient was subjected to resuscitative endovascular balloon occlusion of the aorta in the emergency room before checking for trauma series; however, her blood pressure was temporarily elevated and then decreased despite administering high-dose vasopressor infusion. The hemodynamics of the second patient was constantly aggravated with high-dose vasopressor infusion. Subsequently, both patients died in 90 and 56 min, respectively, after their arrivals. The cross-table lateral radiograph of the cervical spine of both the patients showed atlanto-occipital dislocation (AOD) (Figs. 1 and 2.).
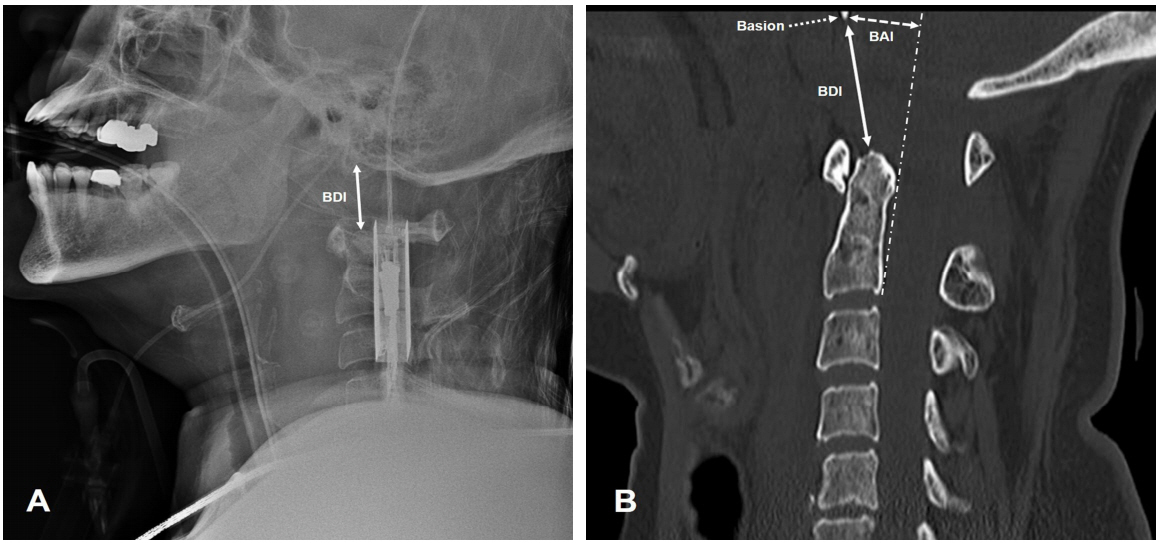
Lateral radiography (A) and computed tomography (B) of the cervical spine demonstrating atlanto-occipital dislocation with 25-mm basion-dental interval (BDI, white arrow) and 16-mm basion-axial interval (BAI, white dotted arrow) and prevertebral hematoma in a 67-year-old woman.
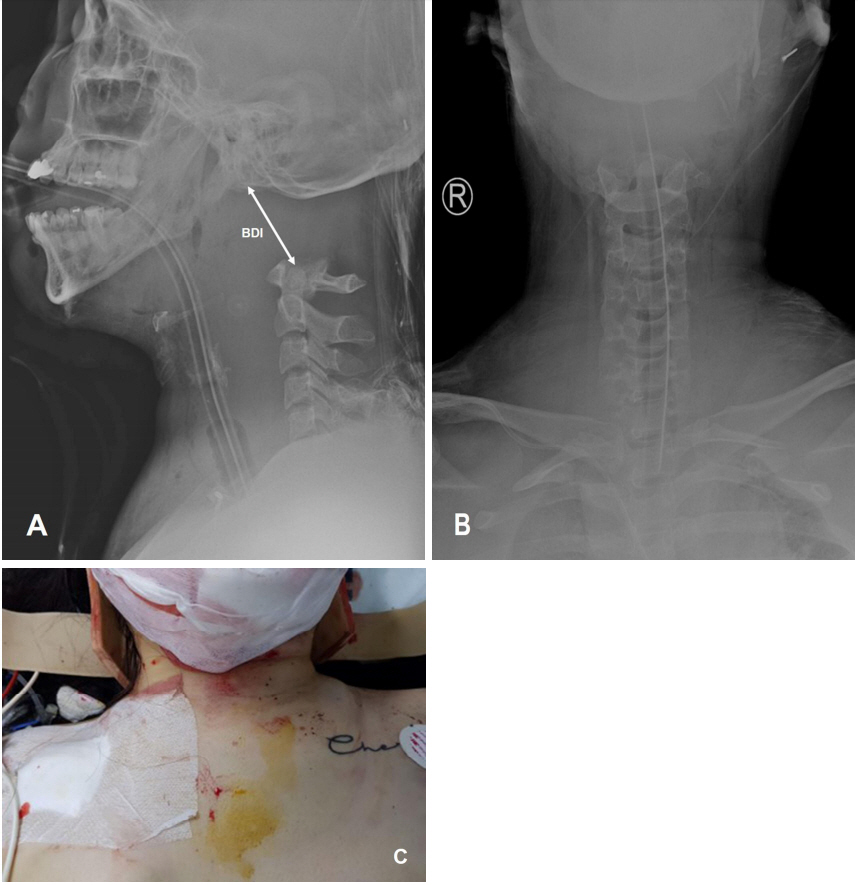
Lateral radiography (A) and anteroposterior radiography (B) of the cervical spine demonstrating atlanto-occipital dislocation with 48-mm basion-dental interval (BDI, white arrow) and floating skull in a 29-year-old woman. (C) An external photograph revealing the swelling of the neck with the application of a cervical collar at the trauma scene.
DISCUSSION
According to the Traynelis classification, AOD can be categorized into Type I (anterior displacement of the occiput to the atlas), Type II (distraction), and Type III (posterior displacement) dislocations [1]. Various radiographic and descriptive features have been proposed for the diagnosis of AOD. Of these, the Harris method with the basion-dental interval (BDI) and basion-axial interval (BAI) are commonly used owing to their relative diagnostic accuracy. The BDI and BAI measures the distances between the basion and the tip of the dens and between a line drawn tangentially to the posterior cortical surface of C2 and a second parallel line drawn through the basion, respectively [2-3]. Values of BDI or BAI >12 mm indicate AOD. The BDI is particularly sensitive to Traynelis type II dislocation, whereas BAI is sensitive to Traynelis type I and III. As all these cases were classified as Traynelis type II dislocation, their BDI’s were 25 mm and 48 mm, respectively. A BDI of ≥16 mm or AOD with neurological deficit is associated with mortality [4].
Notes
Conflict of Interest Statement
No potential conflict of interest relevant to this article was reported.