Right Hemihepatectomy after Damage control Surgery for High-grade Hepatic Injury with Diaphragm Rupture
Article information
Abstract
Liver resection is believed to play a minimal role in the management of hepatic injury because of the high morbidity and mortality associated with it. However, the staged management of high-grade hepatic injuries with anatomic or nonanatomic resection can be accomplished with low mortality and morbidity after a successful damage control surgery. Here, we describe a case of successful major liver resection performed in stages after damage control surgery with effective perihepatic packing in a 40-year-old male with high-grade hepatic injury and diaphragm rupture following crushing thoracoabdominal trauma.
CASE
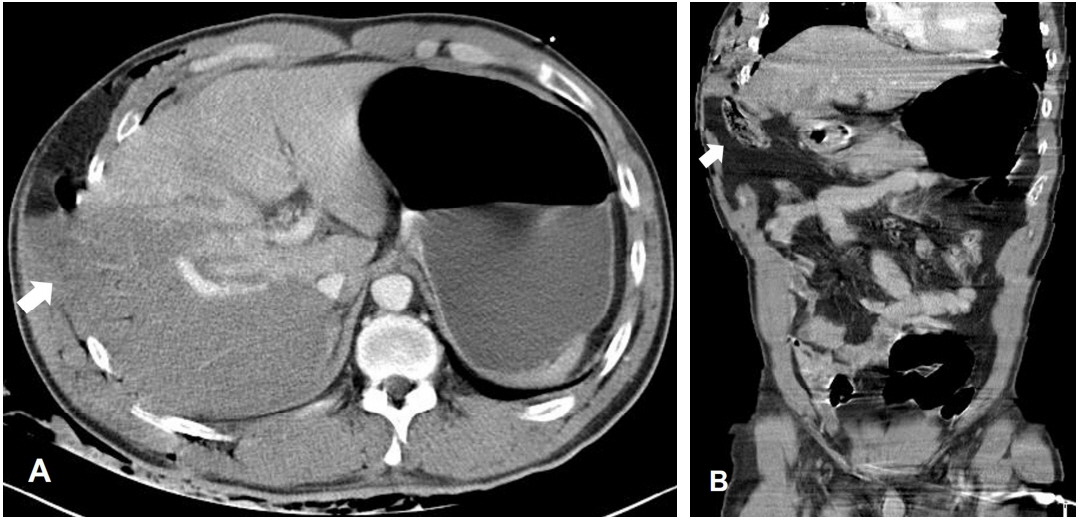
A 40-year-old male was admitted with penetrating and blunt injury to his right thoracoabdominal area caused by a crushing accident at his workplace (Fig. 1.). Upon admission, he was alert with a blood pressure of 135/81 mm Hg, pulse rate of 109 beats/min, respiratory rate of 40/min, and hemoglobin level of 8.5 g/dL. Physical examination revealed peritoneal irritation signs on the whole abdomen. A focused assessment with sonography for trauma revealed large amounts of intra-abdominal fluid collection in the Morison pouch and splenorenal recess. Computed tomography performed in response to resuscitation demonstrated a right hepatic injury and a right diaphragm rupture with herniation of the colon (Fig. 2.). He underwent emergency laparotomy, including primary repair of the right diaphragm, perihepatic packing, and temporary abdominal closure, with an operation time of 84 min (Video 1.). After the damage control surgery, a lethal triad with a pH of 7.26, lactate level of 4.3 mmol/L, international normalized ratio of 2.40, and a temperature of 35.1°C occurred and was corrected after resuscitation of transfusion and warming in the intensive care unit (ICU). Definitive surgery, including right hemihepatectomy and definitive abdominal closure, was performed 12 h after the first operation (Video 2.). The patient was discharged without any complications 20 days after the definitive surgery.

External photographs revealing a penetrating wound in the right lower chest with herniation of the omentum
DISCUSSION
Patients with high-grade hepatic injury are susceptible to the lethal triad of coagulopathy, acidosis, and hypothermia. These patients benefit from damage control resuscitation and physiological restoration in the ICU. Perihepatic packing as a damage control surgery can be used to tamponade and control hepatic hemorrhage and thereby abbreviate the operation [1]. A planned reoperation after the damage control surgery for hepatic injury has been reported to result in better survival rates and fewer infectious complications with perihepatic packing and appropriate antibiotics rather than with anatomical resection of the liver in an acute setting [2].
Because this case was that of a penetrating injury with a diaphragm rupture, despite stable hemodynamics, surgical management had to be primarily considered rather than angiographic intervention. As this patient showed grade V laceration according to the liver injury scale of American Association for the Surgery of Trauma, it was obvious that an initial anatomic resection could result in death, whereas effective perihepatic packing could lead to a definitive surgery with physiological stabilization even for major hepatic injury.
Notes
Conflict of Interest Statement
None of authors have a conflict of interest.
Supplementary materials
Video 1.
A video recording of the damage control surgery with primary repair of the right diaphragm, perihepatic packing, and temporary abdominal closure
Video 2.
A video recording of the definitive surgery with right hemihepatectomy and definitive abdominal closure after the damage control surgery