Modified unilateral inguinal incision preperitoneal packing in a patient with an unstable pelvic bone fracture with ongoing abdominal wall hemorrhage
Article information
Abstract
Pelvic bone fractures may be life-threatening and often requires surgical intervention such as preperitoneal packing or angiographic intervention as hemorrhagic shock progresses. Abdominal wall hematoma due to blunt trauma is uncommon, but in case of hemodynamic instability or growing hematoma, surgical intervention is required. Here we reported the case of a patient who had both unstable pelvic bone fracture and abdominal wall hematoma with hemorrhagic shock.
Introduction
Preperitoneal pelvic packing (PPP) is useful in patients with hemodynamically unstable pelvic fracture and has considerably reduced the amount of transfusions and mortality in high-risk patients [1]. Usually, PPP utilizes either midline incision or Pfannenstiel incision [2].
Depending on the traumatic energy vector, pelvic fracture may be accompanied by abdominal wall hemorrhage. Surgical or angiographic intervention is indicated in hemodynamically unstable patients with growing hematoma [3-5]. We reported the case of a patient diagnosed with both pelvic fracture and abdominal wall hemorrhage who underwent unilateral PPP via inguinal incision.
Case presentation
A 39-year-old male traffic accident victim was transferred to our trauma center. The patient had a clear mental status but complained of severe hip pain. The patient’s blood pressure was 97/37 mmHg and heart rate was 82/minute upon arrival. The right lower abdomen was swollen, and it continued to increase in size (Fig. 1). Abdominopelvic computed tomography revealed the complete disruption of his right sacroiliac joint, right superior and inferior ramus fractures with hemorrhagic fluid collection, and extravasation of contrast anterior to the right lower rectus sheath (Fig. 2). The patient’s initial hemoglobin was 14.0 g/dL (normal range, 13.5-17.0 g/dL), international normalized ratio of prothrombin time was 1.15 (normal range, 0.92-1.13), and lactate was 2.52 mmol/L (0.5-2.0 mmol/L). Two units of packed red blood cells (pRBC) were transfused; however, the patient’s blood pressure was 91/55 mmHg and heart rate was 88/minute. We decided to perform surgical intervention rather than angiography because the radiologist was not ready.

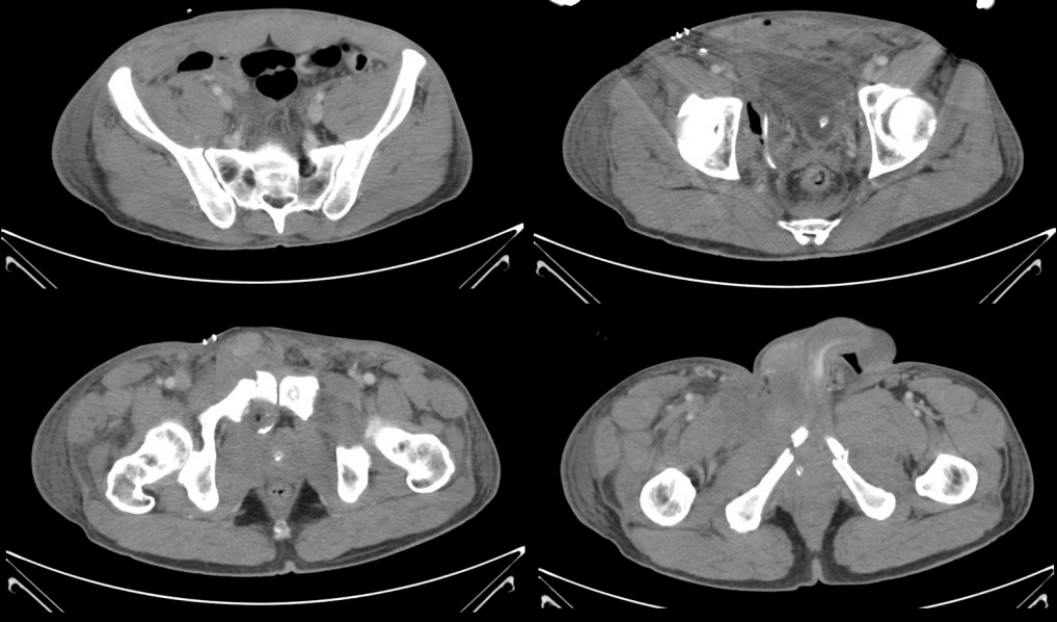
Abdominopelvic CT: (A) disruption of the right sacroiliac joint and rectus sheath hematoma is observed, (B-D) extravasation of contrast in the rectus sheath, right rami fractures, and hematoma from the pelvic bone is observed.
Before the operation, we suspected that the main hemorrhagic focus was the inferior epigastric artery (IEGA) or femoral artery (FA). Subsequently, inguinal incision was performed to identify the hemorrhagic focus, with PPP as a secondary option. A large amount of hematoma in the subcutaneous tissue was evacuated. The detachment of connective tissue and muscle from the pelvic cavity wall permitted easy FA access. Small innominate vessels with active hemorrhage were ligated, but unexpectedly, no hemorrhage in IEGA and FA was observed. Instead, massive hemorrhage recurred from the pelvic bone as pressure around the pelvic cavity decreased. As hemorrhage persisted, we revised the plan to perform unilateral PPP without additional incision because the pelvic bone fracture was confined to the right side. Furthermore, 12 sponges were packed into the preperitoneal space of the right pelvic cavity (Fig. 3) and the incision was temporarily closed to plan for the second-look operation. In total, 10 units of pRBC and 8 units of fresh frozen plasma were transfused on the day of operation.
Further, 45 hours after the first operation, the second-look operation was performed. Previously packed sponges were removed; no additional hemorrhage was observed from the pelvic cavity and abdominal wall. Detached pelvic cavity wall muscles could not be repaired, but other abdominal wall muscles were not damaged, so there was no risk of abdominal hernia. After closed reduction and external fixation for the pelvis, the incision was completely closed (Fig. 4).
Abdominopelvic CT after the second-look operation. The pelvic bone was fixed, and no additional hemorrhage was observed.
The patient’s vital signs were stabilized, and he was discharged from the intensive care unit (ICU) after 3 days (ICU days, 7 days). Subsequently, the patient underwent additional surgery for pubic symphysis and right ramus fracture and an additional midline incision was made (Fig. 5).
Discussion
PPP or angiographic intervention is performed for hemodynamically unstable pelvic fractures [6,7]. Abdominal wall hemorrhage in blunt trauma is common. Hemodynamically unstable fractures or growing hematomas are indications for surgical or angiographic intervention [3,5]. In our case, continuing hemorrhage was confirmed, so surgical or angiographic intervention was essential. We selected surgery instead of angiography because the radiologist was not ready and owing to the requirement of evacuation of the large and growing hematomas.
We selected inguinal incision to access the right IEGA and FA because PPP was a secondary option. After we decided to perform PPP, an additional midline incision was not selected because the major hemorrhagic focus and pelvic bone fracture were limited to the right side. Consequently, the patient could be successfully treated using unilateral inguinal incision PPP. The advantage of inguinal incision PPP is that it provides easy access to large vessels in the inguinal area and bleeding from the abdominal wall in patients with a localized injury.
However, PPP requires additional orthopedic surgeries. Because various incisions can be made depending on the type of pelvic bone fracture, our orthopedic surgeon selected inguinal incision.
Based on our experience with this case, modified unilateral inguinal incision PPP can be a treatment option in patients presenting with unilateral pelvic bone fracture and hemorrhage.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.


