Central venous catheterization into the femoral vein
Article information
Abstract
A central venous catheter (CVC) is usually placed to replace the spilled blood volume or inject a vasopressor. Among central catheterizations, the anatomy of the femoral vessel is lesser complex than that of others, and femoral venous catheterization is most easily cannulated percutaneously. However, endovascular training should be considered to complete the deployment of the central catheter and prevent complications systematically. Therefore, this study aimed to share the precise CVC procedure in the femoral vein and to impart endovascular techniques through simulation video clips and pictures.
The technique of central venous catheterization (CVC) into the femoral vein
To place the femoral venous catheter, the anatomy should be understood first. The femoral vein is located medial to the femoral artery in the femoral sheath and inferior to the inguinal ligament [1]. The inguinal ligament courses between the anterior superior iliac spine (ASIS) and pubic tubercle (Fig. 1). Ultrasound guidance can be used to identify the femoral vessels and reduce the number of cannulation attempts and mechanical complications [2-4]. If there is excess hair, it may be clipped but not shaved from the puncture site. Because shaving increases the risk of infection. Prescan shows vascular anatomy to decide whether a site is suitable for catheterization, and the vein is easily compressed by the ultrasound probe (Fig. 2) [1]. After identifying the anatomy, the needle should be carefully advanced into the target vessel until it becomes visible on the screen or the return of blood is visible from the syringe [2,3]. An important point should be noted at this time. The femoral vein should not be punctured above the inguinal ligament. This is not a femoral vein, but an external iliac vein, a non-compressible vessel [1].
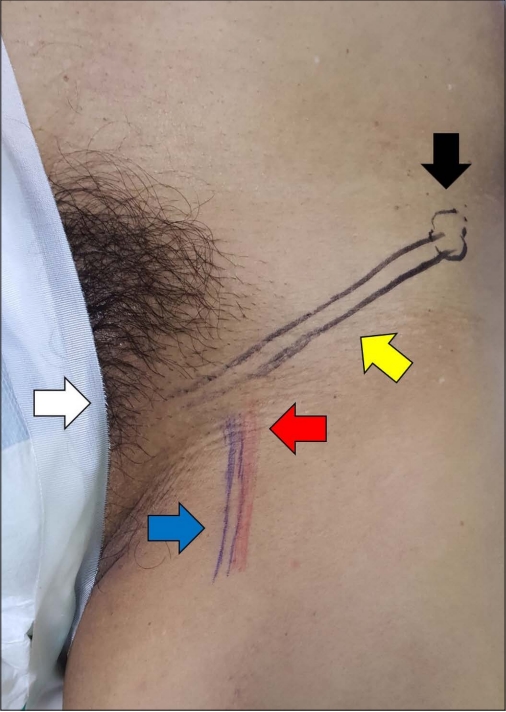
Femoral surface anatomic landmarks; anterior superior iliac spine (ASIS) (black arrow), pubic tubercle (white arrow), inguinal ligament (yellow arrow), femoral artery (FA) (red arrow), and femoral vein (FV) (blue arrow).
Once the vein was accessed, the needle should be stabilized in position with the other hand, and then the guidewire can be advanced approximately 15-20 cm without any resistance [1,2]. After inserting the guidewire, the puncture needle and syringe should be removed. Moreover, a small stab skin incision adjacent to the guidewire using the number 11 blade facilitates the insertion of the dilator along the guidewire [1]. Before inserting the dilator, the end of the guidewire is held by another hand while advancing the dilator, and a dilator should be gently advanced over the wire into the vessel. The dilator is then removed, and the insertion site is gently pressed to avoid excessive blood loss, hematoma formation, and guidewire damage.
When the guidewire appears through the brown opening of the catheter, the end of the guidewire is held by the opposite hand. The venous catheter is advanced over the guidewire into the femoral vein and stepwise advanced the entire length of the femoral catheter hub. When the catheter is properly inserted, the guidewire can be removed from the catheter. A trace of blood should be visible from each port, followed by subsequent flushing with sterile saline to verify the function and clean the line [1,4]. The catheter is anchored to the skin with nonabsorbable sutures, and a sterile dressing is applied. A pelvic X-ray may help confirm the catheter placement (Fig. 3).
All procedures were recorded at the trauma center from Dankook University Hospital (Video) and based on central catheterization using the ARROW® CVC (Arrow, Zdar, Czech Republic).
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Supplementary material
Supplementary data including one video can be found with this article online at www.traumaimpro.org.
Video 1.
A video recording shows central venous catheterization into the femoral vein.

